Introduction
Obesity has emerged as a significant public health concern in the United States, with profound implications for various aspects of health, including urological well-being. This article delves into the correlation between obesity and urological health among American males, highlighting the outcomes of a prospective study that examined the effects of weight management interventions. By understanding these connections, healthcare providers can better tailor interventions to improve the quality of life for affected individuals.
The Prevalence of Obesity in American Males
Obesity is a widespread issue in the United States, with recent statistics indicating that over 40% of American adults are obese. Among males, the prevalence is particularly concerning, as it not only affects overall health but also has specific implications for urological conditions. The increased body mass index (BMI) associated with obesity can lead to a range of urological issues, including urinary incontinence, erectile dysfunction, and an increased risk of kidney stones.
Urological Health and Obesity: A Complex Relationship
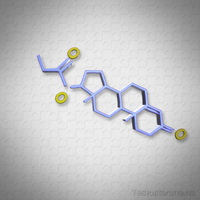
The relationship between obesity and urological health is multifaceted. Excess adipose tissue can lead to hormonal imbalances, such as increased estrogen levels, which can adversely affect prostate health. Additionally, obesity is a known risk factor for type 2 diabetes, which can further exacerbate urological issues by contributing to nerve damage and poor blood flow. These factors collectively underscore the need for targeted interventions to mitigate the impact of obesity on urological health.
Prospective Study on Weight Management Interventions
A recent prospective study conducted on a cohort of American males aimed to evaluate the effectiveness of weight management interventions on urological health outcomes. The study included participants with a BMI of 30 or higher and tracked their progress over a 12-month period. Interventions included dietary modifications, regular physical activity, and, in some cases, bariatric surgery.
Findings: Improved Urological Health with Weight Loss
The results of the study were promising. Participants who achieved significant weight loss reported improvements in various urological health metrics. For instance, there was a notable reduction in the incidence of urinary incontinence and erectile dysfunction among those who lost at least 10% of their initial body weight. Furthermore, the study found a decreased risk of developing kidney stones in participants who maintained their weight loss over the study period.
Mechanisms Behind the Improvements
The improvements in urological health observed in the study can be attributed to several mechanisms. Weight loss leads to a reduction in visceral fat, which in turn can improve insulin sensitivity and reduce inflammation. These changes can positively affect hormonal balance and blood flow, both of which are crucial for maintaining urological health. Additionally, the psychological benefits of weight loss, such as improved self-esteem and reduced stress, can also contribute to better urological outcomes.
Implications for Clinical Practice
The findings of this study have significant implications for clinical practice. Healthcare providers should prioritize weight management as a key component of urological care for obese American males. This approach involves not only recommending lifestyle changes but also providing support and resources to help patients achieve and maintain their weight loss goals. In cases where lifestyle modifications are insufficient, bariatric surgery may be considered as a viable option.
Conclusion
The correlation between obesity and urological health in American males is a critical area of focus for healthcare professionals. The prospective study discussed herein underscores the potential benefits of weight management interventions in improving urological outcomes. By addressing obesity through comprehensive and personalized approaches, it is possible to enhance the quality of life for many American males struggling with urological health issues. As research continues to evolve, it is imperative that healthcare providers stay informed and proactive in their efforts to combat the dual challenges of obesity and urological health.
Contact Us For A Fast And Professional Response

- Urological Health and Sexual Wellness: A Comprehensive Guide for American Men [Last Updated On: March 8th, 2025] [Originally Added On: March 8th, 2025]
- Hydration's Vital Role in Urological Health for American Males [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Genetic Insights into Prostate Cancer, BPH, and Kidney Disease in American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Managing Urological Pain: Causes, Diagnosis, and Treatment Strategies for Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Urological Infections in Men: Causes, Prevention, and Management Strategies [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Urological Health Strategies for American Men in the Workplace [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Heart and Urology: Interconnected Health in American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Urological Health and Fertility: Conditions, Diagnosis, and Management for American Males [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Urological Innovations Enhancing Care for American Males: Trends and Advancements [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Exercise Routines to Enhance Urological Health in American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Smoking's Detrimental Effects on Urological Health in American Men [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Urological Health Guide for American Men: Symptoms, Detection, and Management [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Urological Health Essentials for American Males: Screenings, Lifestyle, and Education [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Urological Health Essentials for American Male Athletes: Risks, Prevention, and Care [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Understanding Urological Insurance Coverage: A Guide for Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Debunking Urological Myths: Facts on Prostate Cancer, Urination, and Erectile Dysfunction [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Specialized Urological Care and Services for American Veterans [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Urological Health's Psychological Impact on American Men: Addressing Stigma and Support [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Urological Health in Aging Men: Screening, Lifestyle, and Advances in Treatment [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Stress and Urological Health in American Males: Impacts and Management Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Dietary Strategies for Enhancing Urological Health in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Supplements and Urological Health: A Guide for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Obesity's Impact on Urological Health in American Men: Risks and Mitigation Strategies [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urological Health in Young American Males: Importance of Early Detection and Screening [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urological Surgery Recovery Guide for American Males: Tips and Strategies [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urological Health and Cancer: Risks, Prevention, and Early Detection in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urological Health's Impact on Mental Well-being in American Men: A Holistic Approach [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Urological Health: Essential Preventive Care for American Men's Well-being [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Urological Health in American Men: Conditions, Prevention, and Holistic Care [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Urological Health: Key to Fertility and Family Planning for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Environmental Factors Impacting Urological Health in American Males: Risks and Prevention [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Urological Health and Sleep Quality: A Vital Connection for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Urological Health: Essential Travel Tips for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health Guide: Procedures, Diagnosis, and Care for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Rehabilitation: Enhancing Urinary, Sexual, and Prostate Health for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Empowering Men: Integrating Urology into Sexual Health Education in the U.S. [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health and Immunity: Strategies for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health: Key to Longevity for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Technological Advances in Urological Diagnosis for American Males: Imaging, Minimally Invasive Procedures, and Beyond [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Exercise Benefits and Safe Practices for Urological Health in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Medications' Impact on Urological Health in American Men: A Comprehensive Overview [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Optimizing Urological Health: Best Practices for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Urological Health's Impact on American Men's Social Life and Well-being [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Alcohol's Impact on Urological Health: Risks and Strategies for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Integrating Urological Health into U.S. Men's Health Campaigns: A Vital Step Forward [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Urological Health and Vision: Exploring Connections and Impacts in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Urological Health in American Men with Chronic Illnesses: Strategies and Insights [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Urological and Bone Health Link: Essential Insights for American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Urological Health Impact and Management Strategies for American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Urological Health's Impact on Mental Well-being in American Men: Awareness and Management [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Urological Health and Skin Care: A Vital Connection for American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Urological Health and Hearing Loss: Vascular, Hormonal, and Inflammatory Links in American Males [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Urological Health: Vital for Men's Well-being and Advocacy in the U.S. [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Urological Health in American Men: Research, Impact, and Future Directions [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Urological Health Linked to Dental Care: Implications for American Men's Well-being [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Urological and Respiratory Health Link in American Males: Importance and Impact [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Urological and Digestive Health: Interconnected Systems and Holistic Care for American Males [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Urological Health's Impact on American Men's Careers: Management Strategies [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Urological and Endocrine Health: A Vital Connection for American Males [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Urological Health in U.S. Men's Policy: Need for Focus and Reform [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Urological Health: Breaking Stigma, Enhancing Men's Well-being in America [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Urological and Musculoskeletal Health: A Holistic Guide for American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Urological and Cardiovascular Health: Critical Links and Management for American Males [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Urological Health in American Males: The Critical Neurological Connection [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Urological Health in American Men: Conditions, Screenings, and Lifestyle Impact [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Urological Health Integration in U.S. Men's Programs: Importance and Impact [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Urological Health's Impact on American Men's Family Life and Well-being [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Urological and Reproductive Health: Essential Connections and Care for American Men [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Enhancing Men's Health: The Critical Role of Urological Care in the U.S. [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Urological Health: Vital for Men's Well-being and Advocacy in the U.S. [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Urological Health Essentials for American Males: Prevention and Care Strategies [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Urological Health's Impact on American Men's Community Involvement and Proactive Care [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Urological Health and Emotional Well-being in American Men: A Holistic Approach [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Urological Health's Impact on American Men's Social Well-being: Insights and Strategies [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Urological Health and Immune Function: A Vital Connection for American Males [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Enhancing Men's Health: Integrating Urological Education into American Programs [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Urological Health and Mental Well-being: A Holistic Approach for American Males [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Urological Health Crucial for American Males' Well-being and Quality of Life [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- Urological Health's Impact on American Men's Life Quality: Insights and Strategies [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]
- Prostate Cancer in American Males: Understanding, Detection, and Advanced Treatments [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]