Introduction
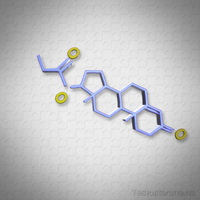
Hypogonadotropic hypogonadism (HH) is a condition characterized by inadequate gonadotropin-releasing hormone (GnRH) secretion from the hypothalamus, leading to decreased production of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) by the pituitary gland. This hormonal imbalance results in diminished testosterone levels and impaired spermatogenesis, significantly affecting the quality of life of young American men. Two primary treatment modalities for HH are human chorionic gonadotropin (hCG) monotherapy and exogenous testosterone replacement therapy. This article delves into the comparative outcomes of these treatments on testicular function, specifically tailored to the needs and concerns of young American males.
Understanding Hypogonadotropic Hypogonadism
HH can be congenital or acquired and manifests through symptoms such as decreased libido, erectile dysfunction, infertility, and reduced muscle mass. For young men in America, where societal expectations often emphasize physical prowess and fertility, HH can be particularly distressing. The choice of treatment, therefore, is not only a medical decision but also one that impacts psychological well-being and life quality.
hCG Monotherapy: Mechanism and Benefits
hCG is structurally similar to LH and can stimulate Leydig cells in the testes to produce testosterone. When used as a monotherapy for HH, hCG has the advantage of preserving or even enhancing spermatogenesis, a critical factor for young men who wish to maintain or regain fertility. Studies have shown that hCG can increase intratesticular testosterone levels, which are essential for spermatogenesis, without the suppression of endogenous gonadotropin production that can occur with exogenous testosterone.
Exogenous Testosterone Therapy: Efficacy and Limitations
Exogenous testosterone therapy is effective in rapidly increasing serum testosterone levels, thereby alleviating symptoms of hypogonadism such as fatigue and decreased libido. However, this treatment can lead to the suppression of the hypothalamic-pituitary-gonadal axis, potentially causing testicular atrophy and azoospermia, which are significant concerns for young men desiring future fertility. The ease of administration and rapid symptom relief make this a popular choice, yet the long-term implications on testicular function necessitate careful consideration.
Comparative Outcomes on Testicular Function
Research comparing hCG monotherapy with exogenous testosterone in young men with HH indicates that hCG is superior in maintaining testicular volume and supporting spermatogenesis. A study involving young American males with HH demonstrated that those treated with hCG had significantly higher sperm counts compared to those receiving exogenous testosterone. Furthermore, hCG treatment was associated with a more favorable lipid profile and less impact on bone mineral density, both of which are crucial for long-term health.
Patient-Centric Considerations
For young American men, the decision between hCG monotherapy and exogenous testosterone involves weighing immediate symptom relief against long-term health and fertility goals. hCG offers a more natural approach to restoring hormonal balance and preserving fertility, which aligns with the aspirations of many young men who envision starting a family. Conversely, the convenience and rapid effectiveness of exogenous testosterone may be more appealing to those prioritizing immediate symptom alleviation over fertility.
Conclusion
In managing hypogonadotropic hypogonadism in young American men, both hCG monotherapy and exogenous testosterone therapy have their merits and drawbacks. hCG monotherapy stands out for its ability to support testicular function and fertility, aligning well with the long-term health and life goals of many young men. However, the choice of treatment should be individualized, considering the patient's immediate needs, fertility aspirations, and overall health objectives. As research continues to evolve, it is imperative for healthcare providers to stay informed and guide their patients towards the most suitable treatment options that enhance their quality of life and future well-being.
Contact Us For A Fast And Professional Response

- Optimizing Testosterone Levels: Clomiphene Citrate's Role in Treating Secondary Hypogonadism in American Men [Last Updated On: February 22nd, 2025] [Originally Added On: February 22nd, 2025]
- Multimodal Endocrine Evaluation Crucial for Diagnosing Fatigue in American Men [Last Updated On: February 26th, 2025] [Originally Added On: February 26th, 2025]
- The Impact of Insulin Resistance on Male Hormonal Health: A Comprehensive Overview [Last Updated On: March 7th, 2025] [Originally Added On: March 7th, 2025]
- Optimizing Hormone Therapy: Vitamin D's Role in Androgen Metabolism and HRT Protocols [Last Updated On: March 8th, 2025] [Originally Added On: March 8th, 2025]
- Optimizing Men's Health: Hormonal Balance and Personalized Hormone Replacement Therapy [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- Unveiling the Potential of Neurosteroid Modulation in Treating Stress-Related Endocrine Dysfunction in American Men [Last Updated On: March 12th, 2025] [Originally Added On: March 12th, 2025]
- Harnessing the Power of SARMs: A New Frontier in Treating Male Endocrine Disorders [Last Updated On: March 13th, 2025] [Originally Added On: March 13th, 2025]
- Exploring the Impact of Oxytocin in Male Endocrinology: From Physiology to Therapy [Last Updated On: March 15th, 2025] [Originally Added On: March 15th, 2025]
- Chronobiology's Impact on Male Hormone Rhythms and Clinical Management [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Essential Trace Elements' Impact on Male Hormone Health: Zinc, Selenium, Magnesium [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Mitochondrial Function and Male Hormone Production: Therapeutic Targets for Age-Related Decline [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Precision Medicine in Endocrinology: Tailoring HRT for American Males Using Genomic and Metabolomic Data [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Gut Microbiome's Impact on Steroid Hormone Metabolism in Men: An Endocrinological Perspective [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Metabolomics: Revolutionizing Male Endocrine Health Diagnosis and Personalized Care [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Pharmacogenomics Revolutionizes Hormone Therapy for Men: Personalized Treatment Insights [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Ghrelin Modulation Enhances Testosterone Therapy for Weight Management in Hypogonadal Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Inflammaging and Endocrine Senescence: Impact on Male Hormonal Health and Optimization Strategies [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Adipokines in Male Endocrinology: Testosterone, Insulin Sensitivity, and Therapeutic Insights for American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Pituitary Incidentalomas in Men: Endocrine Evaluation and Management Guidelines [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Endocrine Disrupting Chemicals: Impact on Male Health and Mitigation Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Thyroid-Testicular Axis: Impact on Male Reproductive Health and Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Understanding Male Climacteric Syndrome: Diagnosis, HRT, and Endocrinology's Role [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Optimizing Bone Health in Men on HRT: Importance and Protocols for BMD Monitoring [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Longitudinal Epigenetic Changes from Hormone Replacement Therapy in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Managing Prostate Health During TRT: Risk Stratification and Monitoring Protocols [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Somatostatin Analogues: Versatile Applications in Male Endocrinology and Beyond [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Multimarker Cardiometabolic Risk Assessment for American Males on HRT [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Managing Polycythemia in Men on Testosterone Replacement Therapy: Monitoring and Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Endocrine Reserve Testing in Men: Applications, Limitations, and Clinical Best Practices [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Vasopressin's Role in Male Endocrinology: Therapeutic Applications and Future Research [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Biomarkers in Male Endocrinology: Growth Factors, Cytokines, and Clinical Applications [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Strategic Hormone Optimization to Combat Sarcopenia in Aging American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- OSA in American Men: Beyond Testosterone, Impacting Multiple Endocrine Systems [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Androgen Receptor Sensitivity: Personalizing Hormone Therapy for American Men's Health [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Male Biological Clock: Endocrine Impacts on Fertility and Offspring Health [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Energy Balance and Reproductive Health: Neuroendocrine Integration in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Post-Traumatic Hypopituitarism in American Men: Diagnosis, Treatment, and Lifestyle Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Exercise and Endocrinology: Optimizing Hormonal Health in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing HPT Axis Recovery in American Men Post-Testosterone Therapy: Clinical Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Leptin Resistance in Men: Endocrine Effects and Targeted Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- NAFLD and Male Endocrine Health: Bidirectional Impacts and Management Strategies [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- HRT and Telomere Length: Implications for Aging in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Male Hormonal Health and Cognitive Function: The Role of Hormone Replacement Therapy [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Diurnal Testosterone Fluctuations: Implications for Diagnosis and Hormone Therapy in Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Endocrine Frailty in Aging Men: Multimodal Interventions and Preventive Care Strategies [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Androgen Therapy's Role in Managing Autoimmune Diseases in Men: A Clinical Perspective [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Neuropeptide Y: Key Regulator of Male Endocrine and Metabolic Health [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Free vs. Total Hormones: Key to Accurate Male Endocrinology Diagnosis and Treatment [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Endocannabinoid System's Role in Male Reproductive Endocrinology: Insights and Therapeutic Potential [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Luteinizing Hormone: Key to Male Endocrinology and Fertility Management [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Genetic Insights and Personalized Treatments for Male Hypogonadism [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Subclinical Endocrinopathies in American Men: Diagnosis, Treatment, and Impact [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- INSL3: A Stable Biomarker for Leydig Cell Function and Male Health [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- SHBG's Impact on Male Health: Hormonal Balance, Diagnosis, and Aging [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Endocrine Sequelae of TBI in Men: Long-Term Management and Follow-Up Strategies [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Opioid-Induced Endocrinopathy in Men: Mechanisms, Diagnosis, and Management Strategies [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- AMH's Role in Male Endocrinology: From Infertility to Cancer Diagnostics [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Chemotherapy's Impact on Male Endocrine Function: Monitoring and Intervention Strategies [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Inhibin B: Key Biomarker for Assessing Male Fertility and Endocrine Health in America [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Radiation-Induced Hypopituitarism in Men: Patterns, Diagnosis, and Hormone Therapy [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Hemochromatosis in American Men: Endocrine Effects, Screening, and Management Strategies [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Osteoporosis in Men: Primary, Secondary Types, Endocrine Evaluations, and Treatment Options [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Chronic Kidney Disease: Impacts and Management of Male Endocrine Function [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Hyperparathyroidism's Impact on Male Reproductive Health: Diagnosis and Management Strategies [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Hormonal Dynamics in Male Stress Urinary Incontinence: Insights and Therapeutic Approaches [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Managing Male Sexual Desire Disorders: Hormonal, Psychological, and Therapeutic Approaches [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Optimizing GH and IGF-1 in Male Athletes: Performance, Health, and Ethics [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Adrenal Incidentalomas in American Men: Evaluation, Management, and Long-term Monitoring [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Cushing's Syndrome in Men: Clinical Features, Diagnosis, and Management Strategies [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- HRT and Male Fertility: Current Practices and Future Innovations for American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Androgen Action: Molecular Insights and Endocrine Therapy Advances for American Men [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Enhancing Endocrine Resilience in Men: Hormones, Lifestyle, and Health Strategies [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Hormone Therapy Protocols for Transgender Men: Endocrinology for American Males [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Male Hormonal Contraception: Endocrine Mechanisms and Clinical Progress in American Males [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- AI-Driven Precision Endocrinology: Personalized Hormone Therapy for Men's Health [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]